What are some of the most important things you’ll need to know for IVD clinical trials? Continue reading to learn more.
In-vitro diagnostics (IVD) are tests performed on biological samples, such as blood or tissue, to diagnose or monitor medical conditions. IVD devices are coming out with new and improved features leading to more accurate results than ever.
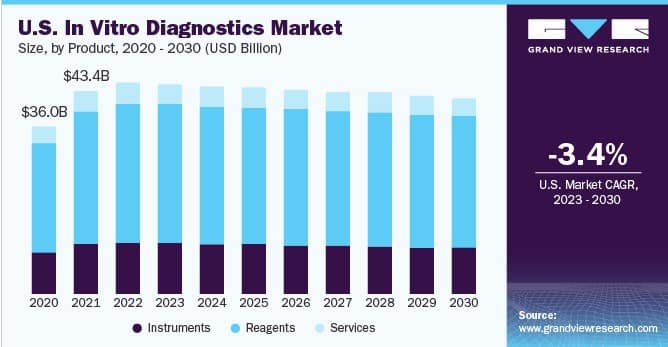
According to a report by Grand View Research, the global IVD market is expected to reach $113.38 billion by 2030, with increasing demand for early disease detection, personalized medicine, and technological advancements driving growth.
However, developing and bringing an IVD device to market often requires extensive clinical trials (or IVD clinical performance studies as referred to in the EU IVDR 2017/746). They should be designed to demonstrate sufficient clinical performance and compliance with the general safety and performance requirements (GSPRs).
Clinical trials play a crucial role in the development and approval of IVD products, but navigating the complex regulatory landscape can be a challenge.
So here we will explore some do’s and don’ts of IVD clinical trials, focusing on key considerations for study design, recruitment, data management, and regulatory compliance. This will lead to better market success for the product. Keep reading to know more.
IVD Clinical Trials: Do’s
Here is what you must consider doing when conducting clinical trials.
1. Develop A Comprehensive Clinical Performance Study Plan
Developing a comprehensive clinical performance study plan is critical to the success of IVD clinical trials. The plan should include the trial’s objectives, design, endpoints, sample size, inclusion/exclusion criteria, and statistical analysis plan. The plan should also indicate the study design type such as observational or interventional and adhere to regulatory requirements.
There should also be a detailed timeline, budget, and risk management plan. This will ensure that the trial is conducted efficiently, safely, and with the necessary regulatory compliance.
2. Prioritize Patient Safety
Patient or participant safety should be the top priority in any clinical study, including IVD clinical performance study. The Clinical Performance Study Plan should include measures to ensure patient safety, such as monitoring adverse events and implementing safety stopping rules.
Patients should be informed of potential risks and benefits before participating in the trial, and their consent should be obtained in accordance with regulatory requirements.
3. Utilize Validated Assays And Methods
Validated assays and methods are essential to ensure the accuracy and reliability of IVD clinical trials. Assays and methods should be validated in accordance with regulatory requirements, and any modifications to validated methods should be properly documented and justified. In essence, the IVDs utilized in clinical performance studies should accurately represent the final product as it is intended for commercial distribution.
Failure to use validated assays and methods can result in inaccurate or unreliable results and will not be accepted by regulatory bodies.
4. Maintain Good Communication With Regulatory Agencies
Maintaining good communication with regulatory agencies throughout the clinical trial process can help ensure the trial’s success. Certain clinical performance studies require an application for authorization to be submitted to the competent authority.
The member state(s) responsible for the authorization may assess several factors, including the statistical approach, study design, sample size, selected comparators, choice of endpoints and others as per article 67 of the EU IVDR.
Unlike in the US, regulatory agencies in the EU (including notified bodies) do not provide guidance on trial design. However, for companion diagnostics there is the possibility for a pre-submission meeting with the European Medicines Agency (EMA) to align on timelines, which is particularly important in co-development scenarios.
Manufacturers should also be transparent with regulatory agencies regarding any issues that arise during the IVDR Clinical Performance Study, such as adverse events or protocol deviations, including substantial modifications.
5. Include Biostatistics
The involvement of biostatistics is pivotal in the design of clinical trials as it aids in determining the trial’s framework, choosing the appropriate sample size, selection of randomization and blinding methods, and data analysis.
You must involve biostatisticians in all stages of a clinical trial, from protocol development to final analysis. Biostatisticians will ensure that the study design is robust, the data collection methods are valid and reliable, and the results are statistically sound.
Put simply, biostatistics helps researchers make accurate inferences from the data and draw valid conclusions.
6. Use Qualified Personnel
The success of IVD clinical trials depends on the expertise of the personnel involved. It’s essential to have a team of qualified professionals, including, where appropriate, physicians, researchers, laboratory professionals and support staff, who have the necessary knowledge and experience to conduct the study safely and effectively.
It’s also important to ensure that all personnel are adequately trained in the study protocol and are aware of their responsibilities and obligations.
7. Maintain Accurate And Complete Documentation
Proper documentation is essential to ensure the quality and integrity of the trial data. This includes study reports, case report forms, and other documents related to the trial.
Make sure to have all the required documentation for the study.
8. Ensure Efficient Data Management
Data management starts with the development of a data management plan that outlines how the data will be collected, stored, and analyzed. During the trial, data must be collected accurately, efficiently, and securely.
The data must also be monitored for quality and completeness. After data collection, it must be entered into a secure database and verified for accuracy.
It must then be analyzed and reported in a timely manner. Data management is crucial in clinical trial design because it ensures that the data generated is accurate, reliable, and can be used to draw valid conclusions.
9. Incorporate User Feedback Into Trial Design And Execution
User input can provide valuable insights into the use experience, including ease of use and comprehension of the IVD device and its instructions for use, as well as potential challenges or concerns. In the contemporary world, feedback is crucial. This area is particularly important for IVDs intended for lay-users and should be available in the technical documentation that is submitted to the notified body.

IVD Clinical Trials: Dont’s
Here is what you should completely avoid doing in the case of IVDR Clinical Performance Studies.
1. Don’t Neglect Regulatory Compliance
IVD clinical trials must comply with regulatory requirements from various governing bodies. In the United States, IVD clinical studies must follow guidelines from the Food and Drug Administration (FDA) for investigational device exemption (IDE) studies.
The European Union has similar requirements for IVD clinical trials, but compliance is overseen by various stakeholders. These include competent authorities, responsible for authorizing the conduct of certain performance studies, Notified Bodies (NBs), tasked with assessing IVD conformity and the European Medicines Agency (EMA) which evaluates companion diagnostics to ensure they are suitable to guide the safe and effective use of medicines. Failure to comply with regulatory requirements can result in delays in approval or even rejection of the device.
2. Don’t Overlook Sample Size And Population Selection
Sample size and population selection are critical components of any clinical trial, including IVD clinical performance studies. A sample size that is too small can result in unreliable results, while a sample size that is too large can lead to unnecessary costs and delays.
Population selection is also crucial, as the trial population should represent the intended use population for the device. Failure to consider sample size and population selection can result in inconclusive or biased results.
3. Don’t Ignore Data Integrity
Data integrity is critical to the validity and credibility of the results of IVD clinical trial, with data management being a key component of ISO 20916. Data should be recorded accurately and completely, and any modifications to data should be properly documented and justified.
Data integrity violations can result in the rejection of the device by regulatory agencies and damage the reputation of the manufacturer.
4. Don’t Rush The Clinical Trial Process
Rushing the IVD clinical trial / clinical performance study process can lead to errors, inaccuracies, and potential safety issues. Manufacturers should allow sufficient time for the trial to be conducted properly, including patient recruitment, data collection, and analysis.
Skipping crucial steps or not taking the time needed for each one can result in incomplete or inaccurate data, leading to inconclusive or misleading results.
5. Don’t Cut Corners On Ethics
Ethical considerations should be at the forefront of IVD clinical trials. This includes obtaining informed consent from study participants in the case of interventional or risky studies for example, ensuring that the study protocol is reviewed and approved by an ethics committee, and adhering to strict guidelines for data collection, analysis, and dissemination.
Cutting corners on ethics can not only compromise the integrity of the trial but also have legal and financial consequences.
6. Don’t Over Promise Results
It’s important not to overpromise results or make false claims about the effectiveness of the product being tested. This not only undermines the integrity of the trial but also puts patients at risk.
It’s essential to be transparent about the limitations of the study and provide accurate information about the product’s potential benefits and risks.
7. Don’t Neglect The Potential Impact Of Regulatory Changes
The regulatory landscape for IVDs is constantly evolving, and it is important to stay up to date on changes that may impact trial design or require additional approvals.
Failure to do so could result in delays or even the need to repeat parts of the trial. This can lead to increased cost and lead time. So, stay on top of what’s changing and have a mechanism to quickly adapt it to the process.
Key Takeaways For Successful IVD Clinical Trials in 2023
Conducting successful IVD clinical studies (or IVD clinical performance studies as defined in the EU) in 2023 requires careful planning, execution, and adherence to regulatory guidelines. As the demand for precision medicine and personalized healthcare continues to grow, the importance of IVDs in diagnostics and patient care will only increase. Therefore, it is crucial to conduct robust and reliable clinical trials to ensure the safety and effectiveness of IVDs.
The IVD industry is constantly evolving, and it is important to stay up to date with the latest developments and best practices to ensure success. By embracing innovation, collaboration, and a patient-centric approach, researchers can help bring safe, effective, and innovative IVDs to market.
The process of planning and conducting IVD clinical trials can be daunting and complex. If you find yourself struggling or experiencing a lack of progress during the research process, we are here to assist you. You can contact us at any stage of development.
FAQ – IVD Clinical trials
What are the regulatory requirements for conducting an IVD clinical trial?
In Europe, the regulatory requirements for IVD clinical trials are set out in the EU In Vitro Diagnostic Regulation (IVDR). IVDR clinical trials must comply with the requirements for clinical performance studies, which are outlined in Annex XIII of the IVDR and some require notification and approval from the competent authority.
IVD clinical studies in the US are subject to regulatory requirements from the FDA. The regulatory requirements can vary. Typically, an Investigational Device Exemption (IDE) is required for investigational IVD devices that are intended to support a significant change to an existing intended use, or for a new intended use that is not yet approved or cleared by the FDA.
However many IVDs are exempt from IDE regulations if they are non-invasive or if the testing is not used as a diagnostic procedure without confirmation by another established IVD.
What are the challenges of IVDR clinical trials?
The main challenges include meeting regulatory requirements, the potential for variability in test results, difficulties in subject recruitment (especially for rare diseases), selecting appropriate study populations and endpoints, and the need to balance cost and time constraints.
However, these challenges can be addressed through careful study design, appropriate statistical analysis, and robust regulatory oversight.

